Hospital use our Machine Reasoning AI to transform or augment complex, human workloads.

The CYC Advantage
As if you had an unlimited quantity of the most qualified and experienced nurses and case managers.

Autonomous
Acuity Leveling/
Charge Capture
Choosing the proper hospital acuity levels used in medical billing can be a challenge for even the most experienced coders or nurses.
- Over-coding can be an invitation for unwanted attention from payer audits and under-coding leads to under-billing for delivered services.
- The process is laborious and fraught with error due to disconnect between nurse responsible for care delivery and nurse responsible for coding.
- Risk avoidance and perverse incentives unconsciously lead nurses to down-level to avoid both internal and payer scrutiny.
With AUTONOMOUS CHARGE CAPTURE, our system automates the data gathering and human logical decision making process and delivers 100% accurate payer and contract specific charges and level codes for earned revenue with supporting criteria and a natural language explanation in case there are questions from supervisors, payers or regulators.
Results:
- Immediate ROI—capture 100% of earned revenue
- Decrease denial rate
- Improve nurse satisfaction and retention
Autonomous
Utilization Review and Denial Management
Utilization Review and Concurrent Denials are labor, time and cognitive-intensive processes that often result in suboptimal financial outcomes for providers. After manual forensics and review, the staff specialist, UR nurses and case managers use logical reasoning to make care, coding and billing decisions.
- Errors, tool biases, and staff shortages can cause care delays, inaccurate billing, denials and cash conversion delays
- Hospital training and guidelines have to be continually updated due to payer changes
With AUTONOMOUS UTILIZATION REVIEW AND DENIAL MANAGEMENT, our system autonomously executes data gathering, status determination, payer submissions, parses denial notifications and creates draft payer submissions – all grounding out in the patient record, transparent, auditable and patient payer plan specific.
Results:
- Increased revenue, reduced denials and shorter cash conversion cycle
- Reduce manual effort for case managers, nurses, physicians and other employees
- Improve employee satisfaction and retention
20%+ under-billing for delivered care due to:

Human
- Human error (e.g. confirmation bias)
- Avoidance of scrutiny

Machine Learning AI
- Replicates human bias and under-billing
- Not explainable, trustworthy or sufficient for regulators
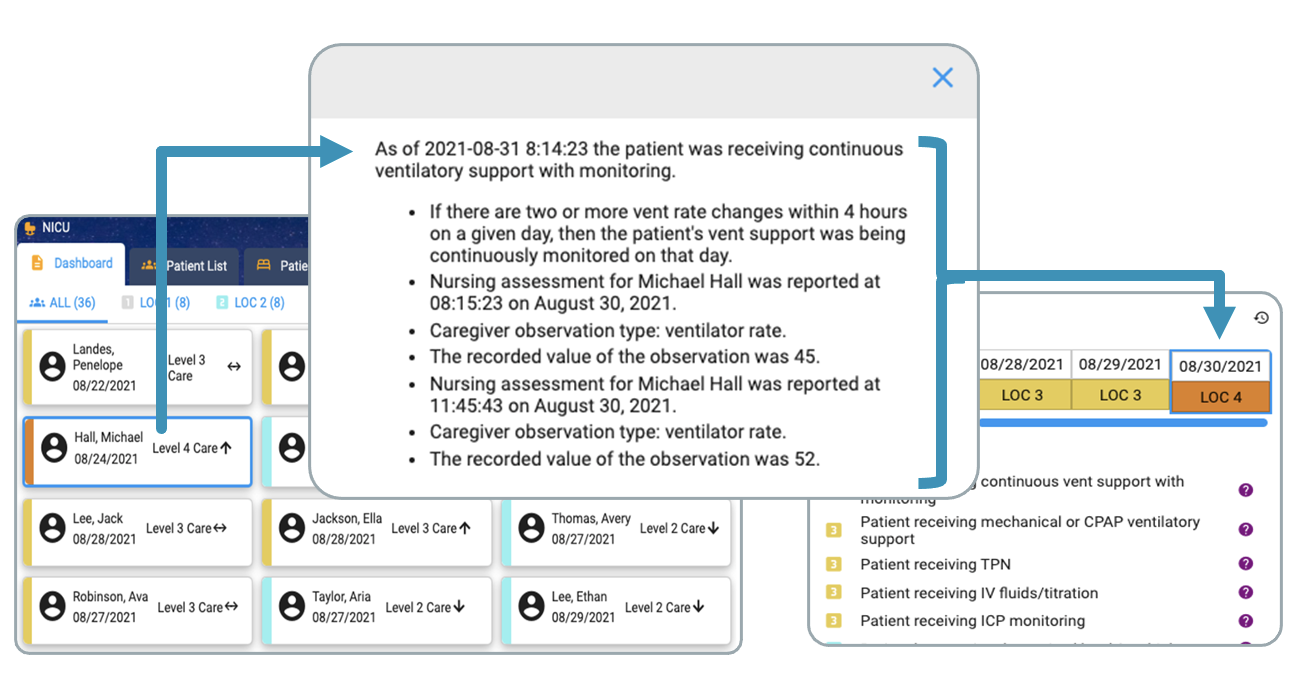
Leveling Module: NICU Example
Key Features / Differentiators
- Autonomous data gathering
- Autonomous logical decision making
- 100% accurate levels and support based on CMS or payer criteria
- Ready to submit to payer
- Explainable, auditable and trusted

Real-time explainable action

ROI for 50-NICU bed hospital
| Avg. Annual NICU days | 12,000 |
| Percent Under Leveled | 20% |
| “Lost dollars”/ patient day | $3,000 |
| Annual Rev Uplift | $7,200,000 |
